The endocervical component in testing or transformation zone (TZ) is an area where the squamous and glandular epithelium meet and is the site of origin for most cervical neoplasia. The TZ may be easily visualized during the clinical examination, or it may be located high within the endocervical canal.
Transformation Zone
The location of the TZ varies from patient to patient, but also may vary in the same individual over time. This may be due to changes in vaginal pH, hormonal changes associated with hormonal therapy or pregnancy, childbirth, menopausal status and bacterial or fungal (candidal) infections.
The presence of the TZ in cervical cytology samples has historically been considered an indicator of specimen quality. This may be due to a 1985 study which examined negative Pap smears, retrospectively. This study showed that a high proportion of Pap smears without a TZ component had a subsequent biopsy diagnosed as cervical intraepithelial neoplasia (CIN) 3, or invasive cancer. This therefore raised the possibility of missing a lesion due to inadequate TZ sampling.
This study was flawed, however, as it did not exclude patients who had an abnormal history and used conventional Pap tests. However, since then, more rigorous studies have shown no increase of abnormalities after a Pap smear without a TZ. (In fact, some studies have found a lower risk of CIN3+ in patients lacking a transformation zone, compared to those with a transformation zone present!)
Adequate Sampling Without TZ
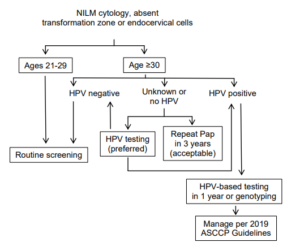
These more recent and accurate studies concluded that early repeat testing is not justified, as there is no increased rate of high-grade lesions evident on longitudinal follow-up. Therefore, the current Bethesda guidelines do not require the presence of TZ for samples to be considered adequate. The ASCCP issued a statement in May of 2021 which echoed this statement and provided guidelines to manage negative Pap tests with an absent TZ. (Please refer to the linked ASCCP statement, and the below diagram.)
These recommendations lean on high-risk HPV testing as a management tool, as it has been shown that high risk HPV detection is independent of the presence or absence of the TZ.
Overall, rescreening cases without a TZ is not value based care (neither cost effective nor necessary.)
 Richard Hopley, M.D. | 06/19/2023
Richard Hopley, M.D. | 06/19/2023